Prostatitis & Prostate Cancer
Prostatitis, Prostate Cancer & Prostate Surgery
Men's pelvic health physiotherapists play a crucial role in assisting men who are dealing with non-bacterial prostatitis (inflammation or swelling of the prostate gland) and recovering from prostate surgery.
Understanding Prostatitis
Prostatitis can cause discomfort and pain in the pelvic region. The most common type is chronic prostatitis (CP) / Chronic Pelvic Pain Syndrome (CPPS). CP and CPPS are clinical syndromes in males defined by pain or discomfort in the pelvic region, often accompanied by urologic symptoms or sexual dysfunction.
CPPS is the most common type of prostatitis, accounting for the majority of cases. It is characterised by long-lasting pelvic pain or discomfort, often accompanied by urinary symptoms such as frequent urination, pain or burning during urination and pain or discomfort in the genitals or lower back.
The exact cause of CP/CPPS is unknown, but it is believed to involve a combination of factors including inflammation, muscle tension and nerve abnormalities.
After Prostate Surgery
Prostate surgery, like a prostatectomy for prostate cancer involves the removal of part or all of the prostate gland and surrounding tissues, which can lead to post-surgical side effects. These side effects range from incontinence, urge frequency, erectile dysfunction and bowel dysfunction.
Our approach is practical and effective
Men's Pelvic Health Physiotherapists are very effective in addressing the specific needs of male patients with CPPS or recovering from prostate surgery by providing specialised care and guidance throughout their journey.
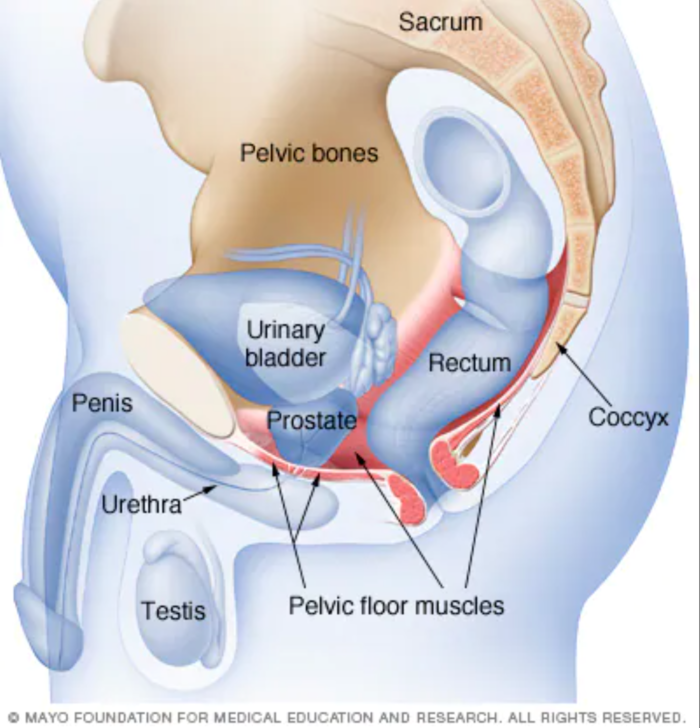
They are able to often alleviate the symptoms of CPPS and side effects of prostate surgery through their in-depth knowledge of the male pelvic anatomy, including the muscles, nerves, and surrounding structures, enabling them to offer targeted interventions and support.
Here are ways in which Men's Pelvic Health Physiotherapists assist men with prostatitis and the side effects of prostate surgery:
Pain Management: Prostatitis can cause pelvic pain, discomfort and sometimes referred pain in the lower back, testicles or groin area. We employ various techniques such as manual therapy, myofascial release and trigger point therapy to alleviate pain and reduce muscle tension in the pelvic region.
Pelvic Floor Muscle Training: The pelvic floor muscles play a vital role in maintaining urinary and sexual function. Specific exercises are taught to strengthen, release when there is tension, and coordinate the pelvic floor muscles with other muscular systems. Coordinated muscle balance assists in managing symptoms related to prostatitis and aids in the recovery process after prostate surgery.
Bladder Training: Prostatitis and prostate surgery can impact bladder function leading to issues such as urinary urgency, frequency or incontinence. Patients learn about bladder training techniques, including timed voiding and urge control strategies to improve bladder control and reduce urinary symptoms.
Bowel Management: Prostate surgery may affect bowel function resulting in changes in bowel habits or constipation. Guidance on bowel management techniques includes dietary modifications, bowel retraining and proper toileting positions to promote regularity and alleviate any associated discomfort.
Scar Tissue Management: Following prostate surgery, the formation of scar tissue is common. Scar tissue mobilisation techniques enhance tissue flexibility, minimise adhesions and improve overall mobility in the surgical area.
Education and Lifestyle Modifications: We offer valuable education regarding lifestyle modifications such as ergonomic advice, proper sitting posture, and strategies to improve overall pelvic health. Concerns or questions you may have about sexual function or activity after prostate surgery are also welcome.